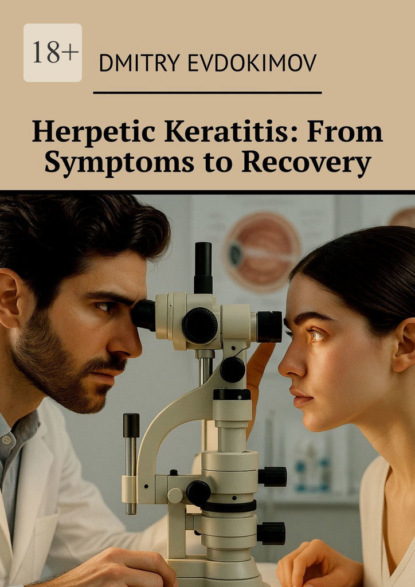
Herpetic keratitis: from symptoms to recovery
- -
- 100%
- +

© Dmitry Evdokimov, 2025
ISBN 978-5-0068-4413-1
Created with Ridero smart publishing system
Herpetic Keratitis: From Symptoms to Recovery
There are contraindications. Consultation with a specialist is necessary.
I would like to express my deepest gratitude to my beloved wife, Anna, whose unwavering help, steadfast support, and boundless patience have been the cornerstone of this book’s completion. Her encouragement and understanding during this demanding journey have been invaluable.
To my son, Nikita, I extend my sincere thanks for his invaluable assistance in editing the tables and diagrams, as well as his thoughtful advice on design matters, which greatly enhanced the clarity and presentation of the material.
I am profoundly thankful to my mother, Nadezhda, whose love and steadfast support provided me with the emotional strength to persevere throughout the writing process.
This book, “Herpetic Keratitis: From Symptoms to Recovery,” would not have been realized without the love, assistance, and encouragement of my family. Their contributions have been deeply cherished and have enriched this work immeasurably.
All rights reserved. No part of this book may be produced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording or any information storage and retrieval system, without permission in writing from the publishers.

Introduction: The Significance of the Problem of Herpetic Keratitis
Herpetic keratitis (Herpes Simplex Virus keratitis) remains one of the most significant causes of infectious blindness worldwide despite advances in modern medicine. Its recurrent nature, complex diagnosis, and need for prolonged treatment make this disease an important topic for ophthalmologists.
Herpetic Keratitis as a Leading Cause of Infectious Blindness
Herpetic keratitis (HK) holds a leading position among infectious causes of vision loss, surpassing bacterial, fungal, and parasitic keratitis. Mechanisms of blindness include:
• Damage to the corneal epithelium and stroma with formation of irreversible scarring.
• Chronic inflammation leading to corneal neovascularization.
• Development of secondary complications such as glaucoma or dry eye syndrome.
1. Statistics:
• According to the World Health Organization (WHO), herpetic keratitis affects more than 1.5 million people globally each year, with approximately 40,000 losing vision in one or both eyes. See Appendix (QR code for Source No. 1)
• In 25% of cases, this disease leads to keratoplasty.
2. Epidemiology: Global Prevalence and Risk Groups
The global prevalence of herpetic keratitis varies depending on the region, healthcare level, and climatic conditions. General indicators:
• HSV-1 infection prevalence among the population reaches up to 90% in some regions, creating a high likelihood of ophthalmic manifestation of the disease.
• Recurrence frequency: more than 25% of patients who experienced the first episode of HK suffer recurrences within the first year, and 50% within 5 years. See Appendix (QR code for Source No. 2)
Risk groups:
• Patients with immunodeficiency conditions (e.g., HIV infection, long-term immunosuppressive therapy, organ transplantation).
– Elderly individuals with reduced regenerative capabilities of corneal tissues.
• Children and young people with a high risk of primary infection.
• Residents of regions with high levels of ultraviolet radiation, as UV exposure activates the virus. See Appendix (QR code for Source No. 3)
Climatic factor:
• Tropical and subtropical countries show a higher frequency of cases associated with viral activation by sunlight.
3. Economic and Social Burden of the Disease
Direct Medical Costs:
Treatment of herpetic keratitis requires substantial resources including:
• Prolonged therapy with antiviral drugs and immunomodulators.
• Repeated physician visits for monitoring.
• Possible surgical intervention (e.g., keratoplasty).
Recent studies indicate the annual direct treatment cost for herpetic keratitis in the United States is approximately $17.7 million, substantially lower than previous estimates. This figure refers specifically to herpetic keratitis and does not include the broader spectrum of herpetic eye disease. See Appendix (QR code for Source No.4)
Indirect Costs:
• Loss of patients’ working capacity, especially during recurrences.
• Work absenteeism and reduced productivity due to the need for regular treatment.
• Social costs including psychological stress related to the chronic nature of the disease.
Quality of Life:
Vision impairment and frequent exacerbations of HK considerably reduce patients’ quality of life, including:
• Limitation of daily activities.
• Fear of vision loss due to recurrences.
•Depression and anxiety disorders associated with prolonged treatment.
Economic burden of herpes:
According to WHO, 2024:
• Annual economic losses from herpes are estimated at $35 billion.
• Genital herpes causes significant healthcare expenses and reduced labor productivity. See Appendix (QR code for Source No. 5)
Conclusion:
Herpetic keratitis is not only a medical but also a socio-economic problem that requires an interdisciplinary approach to treatment and prevention. Its global significance dictates the need to develop new diagnostic, therapeutic, and preventive methods that will reduce disease prevalence and its severe consequences.
Brief Overview of Herpes Simplex Virus (HSV)
Human herpesvirus (Herpes Simplex Virus, HSV) is a widespread DNA-containing virus belonging to the Herpesviridae family. Its unique feature is the ability of latent persistence in the body and reactivation under the influence of external and internal factors. In ophthalmology, two types of the virus play a key role: HSV-1 and HSV-2.
1. Types HSV-1 and HSV-2
HSV-1 and HSV-2 share a similar genetic structure but differ in preferred transmission routes, tissue tropism, and disease spectrum.
HSV-1 (Herpes Simplex Virus Type 1):
Main clinical manifestations:
• Leading cause of ophthalmic herpes: causes epithelial, stromal, and endothelial keratitis, keratouveitis, and recurrent eyelid lesions (herpetic blepharitis).
• Also associated with oral herpes and encephalitis.
Transmission routes:
• Contact: through saliva, skin, mucous membranes.
• Possible transfer to the cornea through contaminated hands or objects (e.g., contact lenses).
Epidemiological significance:
• Over 60% of the adult population worldwide is infected with HSV-1.
• Predominates in countries with temperate and cold climates.
HSV-2 (Herpes Simplex Virus Type 2):
Main clinical manifestations:
• More commonly causes genital herpes but can affect the eyes (e.g., keratoconjunctivitis) in neonatal herpes.
• Less frequently involved in ophthalmic pathology in adults.
Transmission routes:
• Sexual: main mode among adults.
• Vertical: from mother to newborn during childbirth.
Epidemiological significance:
• Occurs in 10—20% of the population depending on the region, more frequent in countries with high HIV prevalence. See Appendix (QR code for Source No. 6)
Comparison of Types:
HSV-1 is more tropic to the trigeminal nerve ganglia and ocular region, whereas HSV-2 mainly affects sacral ganglia. However, both types can affect the eyes and other organs.
2. Mechanisms of Infectivity and Viral Persistence
One of the key features of HSV is its ability for lifelong persistence and periodic reactivation. These properties are explained by unique mechanisms of interaction between the virus and host cells as well as the immune system.
Stages of the Infectious Cycle:
1. Entry into the Epithelium:
– HSV binds to receptors on the surface of epithelial cells, including heparan sulfate proteoglycans (HSPG) and nectin-1 protein.
– The viral capsid is delivered into the nucleus of the cell, where viral DNA is released.
2. Replication and Assembly of Viral Particles:
– The viral genome replicates using host cell enzymes.
– Early and late viral proteins necessary for the assembly of new virions are synthesized.
3. Cytotoxic Effect:
– Lysis of the host cell leads to inflammation and localized tissue destruction, for example, of the corneal epithelium.
Mechanisms of Persistence:
Following primary infection, the virus migrates via sensory nerves to neuronal ganglia, where it can persist in a latent form:
• In the latent phase:
– Viral DNA is maintained in the nucleus of neurons as an episome (circular form, not integrated into host DNA).
– Viral protein synthesis is minimal, rendering the virus “invisible” to the immune system.
• Upon Reactivation:
– Trigger factors (such as ultraviolet radiation, stress, immunosuppression) induce active viral replication and migration back along the nerve pathways to the original site of infection.
3. Zone of Viral Latency in the Trigeminal Nerve
The trigeminal nerve (n. trigeminus) is the key structure where HSV-1 persists in latent form.
• Location: The Gasserian ganglion (ganglion trigeminale) serves as the principal viral reservoir, where the virus resides in a dormant state between recurrences.
• Mechanism of Latency:
– Viral genetic activity remains minimal due to epigenetic control.
– Latency Associated Transcripts (LAT-RNA), which are non-coding RNAs, play a crucial role in suppressing viral replication and maintaining neuronal viability.
• Viral Activation:
– Under the influence of triggers, epigenetic control diminishes, allowing viral replication and migration back to the cornea.
– Repeated activations lead to chronic inflammation and irreversible corneal damage.
4. Modern Aspects of HSV Study
Contemporary research focuses on the latent phase of HSV, prevention of reactivation, and reduction of inflammation-induced damage:
• Molecular Inhibitors:
– New drugs targeted at inhibiting specific viral proteins involved in activation are under development.
• Genome Editing Technologies:
– Use of CRISPR/Cas9 to disrupt the viral genome during latency is being explored.
• Immune Approaches:
– Vaccines capable of eliciting durable cellular immunity against HSV are being investigated.
Conclusion
HSV is a unique pathogen that combines high infectivity, latent persistence, and a recurrent nature.
For ophthalmologists, understanding the mechanisms of infection, latency, and reactivation is essential to selecting optimal strategies for treatment and prevention of herpetic keratitis.
The features of the mechanism of action of herpes simplex virus in the human body are illustrated in Scheme 1.

Chapter 1: Etiology and Pathogenesis of Herpetic Keratitis
Herpetic keratitis (HK) is one of the most common and severe infectious diseases of the cornea caused by the Herpes Simplex Virus (HSV). It develops as a result of the complex interaction between the virus, corneal epithelium, the host immune system, and latent reservoirs of infection. Understanding the etiology and pathogenesis of HK is essential for diagnosis, therapy, and prevention of its complications.
Mechanisms of HSV Infection
1. Routes of Transmission
The Herpes Simplex Virus is transmitted mainly through contact with mucous membranes or damaged skin. The routes of infection depend on the viral type (HSV-1 or HSV-2) and patient age:
• Contact-Domestic Route (mainly for HSV-1):
– Infection occurs via direct contact with affected skin, mucous membranes, or saliva of an infected person.
– Auto-inoculation is possible by transferring the virus from the lips, nose, or other areas to the eye via hands, towels, contact lenses, or cosmetics.
• Sexual Route (typical for HSV-2):
– Virus is transmitted sexually, which less frequently causes ophthalmic herpes but can lead to neonatal infections.
• Vertical Transmission:
– HSV-2 is transmitted from mother to child during childbirth. In newborns, herpetic keratitis is often accompanied by generalized infection.
• Rare Routes:
– Aerosol transmission (possible in laboratory or medical settings).
– Blood transfusion (in exceptional cases).
2. Primary Infection
Primary infection occurs upon the first contact with the virus.
Viral entry:
HSV enters through microtraumas of skin or mucous membranes, binding to specific receptors (nectin-1, HVEM) on the cell surface.
Once inside, the virus releases DNA into the host cell nucleus where viral replication begins.
Clinical features:
Most patients experience a subclinical primary infection without pronounced symptoms.
Ophthalmic manifestations may include acute epithelial keratitis or herpetic conjunctivitis.
Immune response:
Primary infection stimulates innate immunity. Type I interferons (IFN-α, IFN-β) inhibit viral replication, and neutrophils and macrophages destroy infected cells.
After the acute phase, the virus migrates along sensory nerve endings to regional ganglia, where latency is established.
3. Latency and Reactivation
HSV latency is a key mechanism enabling lifelong viral persistence.
Latent infection:
Viral DNA is maintained in the nucleus of trigeminal nerve neurons as an episome, not integrated into host DNA.
Latency is supported by expression of non-coding transcripts (Latency-Associated Transcripts, LAT) that suppress viral replication and block apoptosis of infected neurons.
Triggers of Reactivation:
HSV reactivates under factors disrupting immune control:
• Physical: ultraviolet radiation, eye trauma, surgical interventions.
• Immunological: immunosuppression (e.g., HIV, chemotherapy), viral or bacterial infections.
• Emotional: stress, fatigue.
• Hormonal: hormonal shifts in women, menstruation.
Pathogenesis of HSV Keratitis
1. Corneal Infection (Primary Infection)
The virus penetrates the corneal epithelial cells, causing their destruction:
Viral replication:
• In infected cells, the virus utilizes host mechanisms for reproduction.
• New viral particles are released, infecting neighboring cells.
Cellular damage:
• The cytotoxic effect of the virus leads to the death of epithelial cells and formation of characteristic dendritic ulcers.
Role of the immune system:
• Local activation of innate immunity causes influx of neutrophils and release of pro-inflammatory cytokines (IL-1, TNF-α).
• Immune mechanisms protect against systemic viral spread but may cause additional tissue damage.
2. Chronic Inflammation (Stromal Keratitis)
During reactivation, the virus affects deeper layers of the cornea:
• Immune response:
– Reactivation activates T cells, which infiltrate the stromal layers and trigger production of pro-inflammatory cytokines (IFN-γ, IL-17).
– Antibodies against viral antigens may cause complement-dependent stromal damage.
• Neovascularization:
– Chronic inflammation stimulates growth of blood vessels within the cornea, disrupting its transparency.
• Scarring:
– Fibrosis of the stroma due to inflammation leads to persistent reduction of visual acuity.
3. Endothelial Lesions and Keratouveitis
In severe recurrences, the deep corneal layers and anterior chamber are involved:
• Endothelial keratitis:
– Stromal edema and endothelial damage impair corneal hydration.
• Keratouveitis:
– Anterior chamber inflammation may be accompanied by elevated intraocular pressure and secondary glaucoma development.
Modern Concepts of Pathogenesis
See Appendix (QR code linking to Source No.7)
1. Role of Genetic Predisposition:
• Genetic polymorphisms in immune response genes such as TLR3 and IFNL3 may increase the risk of severe herpetic keratitis.
2. Corneal Microbiome:
• Alterations in the ocular surface microbiota are associated with frequent recurrences.
3. Epigenetic Mechanisms:
• Studies indicate that epigenetic changes in trigeminal nerve neurons can modulate HSV latency and reactivation.
Conclusion
The etiology and pathogenesis of herpetic keratitis involve complex interactions among viral factors, immune response, and host conditions. Deep understanding of these processes allows development of new approaches for treatment and prevention, minimizing recurrence risk and long-term complications.
Stages of the Pathogenesis of HSV Keratitis
Herpetic keratitis is a stepwise pathological condition caused by features of the life cycle of Herpes Simplex Virus (HSV) and the immune system’s response. The pathogenesis is divided into three key phases: latent infection, reactivation, and tissue damage. Each phase is driven by complex interactions between viral factors and host defense mechanisms.
1. Latent Infection
After the primary infection, HSV travels through sensory nerves to regional ganglia where it enters latency.
A) Process of Transition to Latency:
• Virus migration to ganglia:
– After infecting the cornea, the virus is transported via axonal flow into sensory neurons, predominantly the trigeminal nerve (ganglion trigeminale).
– Here, viral DNA remains as an episome, not integrated into the host cell genome.
• Mechanisms of latency:
– During latency, only certain non-coding RNAs called Latency-Associated Transcripts (LAT) are expressed. These transcripts:
• Suppress viral replication.
• Block apoptosis of infected neurons.
• Reduce immune activity around the ganglion.
•Epigenetic modifications of viral DNA play a critical role in regulating its transcription during latency.
B) Immune Control of Latent Infection:
• Latency is maintained by immune surveillance primarily through CD8+ T-cells residing in the ganglia.
• Effector cytokines such as interferon-gamma (IFN-γ) create a microenvironment that inhibits viral reactivation.
2. Reactivation: Triggers and Mechanisms
In the latent state, under certain triggers, the virus reactivates leading to active replication and migration back to the corneal tissues.
A) Major Triggers of Reactivation:
Stress:
• Emotional or physical overexertion activates the hypothalamic-pituitary-adrenal axis, leading to the release of glucocorticoids.
• Stress hormones weaken immune control and increase the likelihood of viral reactivation.
Ultraviolet Radiation (UV):
• UV rays induce localized inflammation and tissue damage.
– There is increased production of pro-inflammatory cytokines such as IL-1 and IL-6, which reduce the activity of immune cells controlling the virus.
• UV radiation also activates MAPK signaling pathways that promote viral replication.
Immunosuppression:
• Immunodeficiency states (e.g., HIV infection, malignancies, chemotherapy) impair cellular immunity, creating conditions for viral reactivation.
• The use of systemic corticosteroids or other immunosuppressants significantly raises the risk of reactivation.
B) Mechanism of Reactivation:
• Reactivation is initiated by suppression of immune control within ganglia, leading to activation of viral replication.
• The active virus migrates back along sensory nerve endings to the cornea, causing tissue damage.
3. Tissue Damage: Viral and Immune Contributions
Tissue destruction in HSV keratitis is caused by two main mechanisms: direct cytotoxic effects of the virus and immune-mediated injury.
A) Cytotoxic Effect of the Virus:
1. Epithelial Cell Destruction:
• HSV replicates in corneal epithelial cells, leading to cell death via necrosis and apoptosis.
• Dendritic and geographic ulcers form as a result of focal epithelial degeneration.
2. Viral Protein Activity:
• The virus encodes proteins that suppress immune responses, such as ICP47, which inhibits antigen presentation on MHC-I.
• US3 and UL41 proteins protect infected cells from apoptosis, prolonging their viability for viral replication.
B) Immune Response as a Source of Damage:
Role of Innate Immunity:
• Neutrophils and macrophages recruited to the infection site release reactive oxygen species and pro-inflammatory cytokines (IL-1, TNF-α).
• This enhances inflammation but also causes collateral tissue damage.
Adaptive Immune Response:
• CD4+ and CD8+ T lymphocytes infiltrate stromal layers of the cornea, provoking chronic inflammation.
• Overactivation of T cells, especially TH1 and TH17 subsets, leads to production of interferon-gamma (IFN-γ) and IL-17, intensifying inflammation.
Fibrosis and Neovascularization:
– Chronic inflammation stimulates corneal neovascularization and fibrous tissue formation, disrupting transparency and reducing vision.
C) Final Pathology:
– In severe recurrences, inflammation may spread to deeper ocular structures (e.g., anterior chamber) causing keratouveitis, increased intraocular pressure, and secondary glaucoma development.
Modern Concepts of Tissue Damage
Genetic Predisposition:
– Polymorphisms in genes such as IL-1B and IFNL3 are associated with the severity of inflammation.
Role of the Microbiota:
– Alterations in the ocular surface microbiome influence the frequency and intensity of recurrences.
Epigenetics:
– Epigenetic modifications of viral and host cellular DNA may determine susceptibility to reactivation.
Conclusion:
The staged pathogenesis of HSV keratitis highlights the importance of viral latency and reactivation triggers as key factors governing recurrences and disease severity. The combination of direct cytotoxic viral effects and an excessive immune response shapes the clinical picture, necessitating a balanced therapeutic approach.
Types of Corneal Involvement in Herpetic Keratitis